- Etiology: prerequisite is malrotation – abnormal rotation of the gut as it returns to the abdominal cavity during embryogenesis -> narrow mesenteric root -> volvulus / twisting of mesenteric pedicle around superior mesenteric artery -> venous obstruction -> continued arterial inflow -> venous congestion -> raised tissue pressure above blood pressure -> cessation of arterial flow / arterial obstruction -> midgut ischemia / necrosis from jejunum to middle of colon
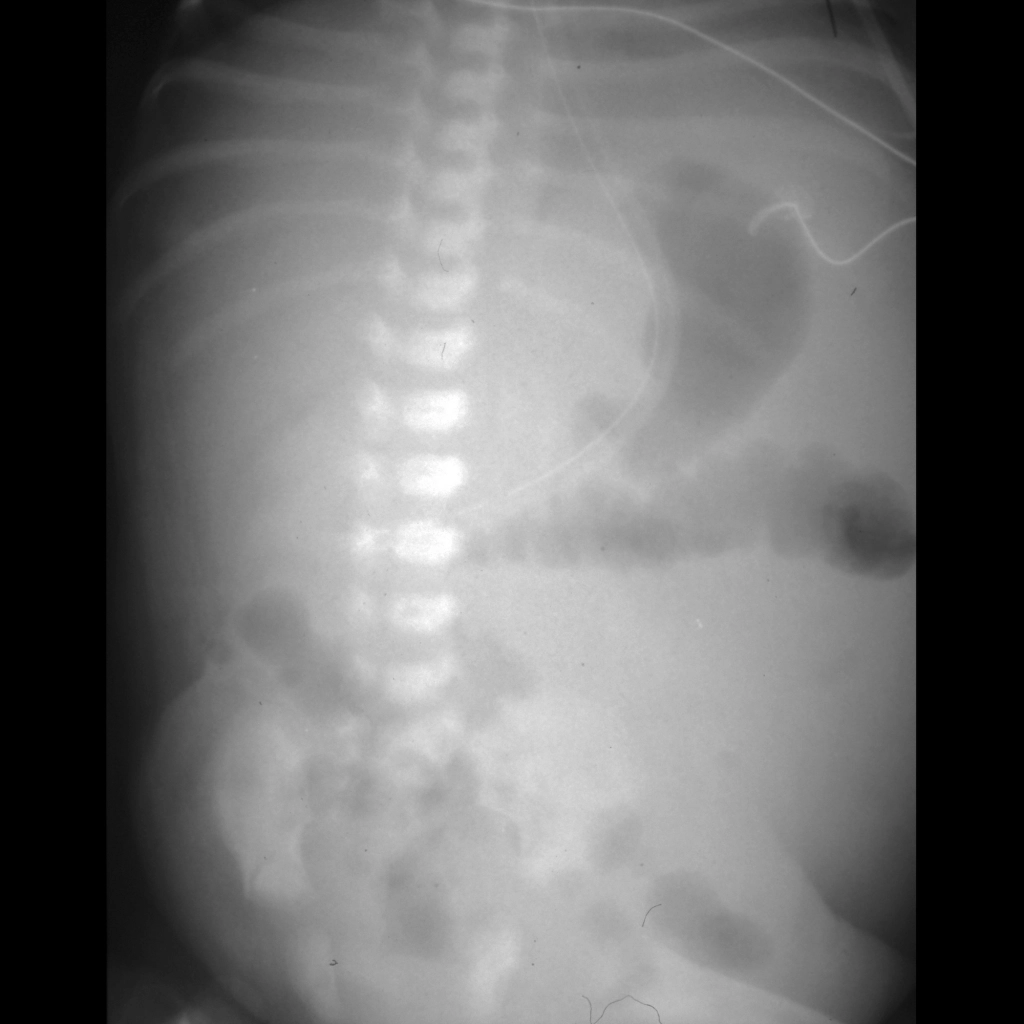
- AXR: usually unremarkable
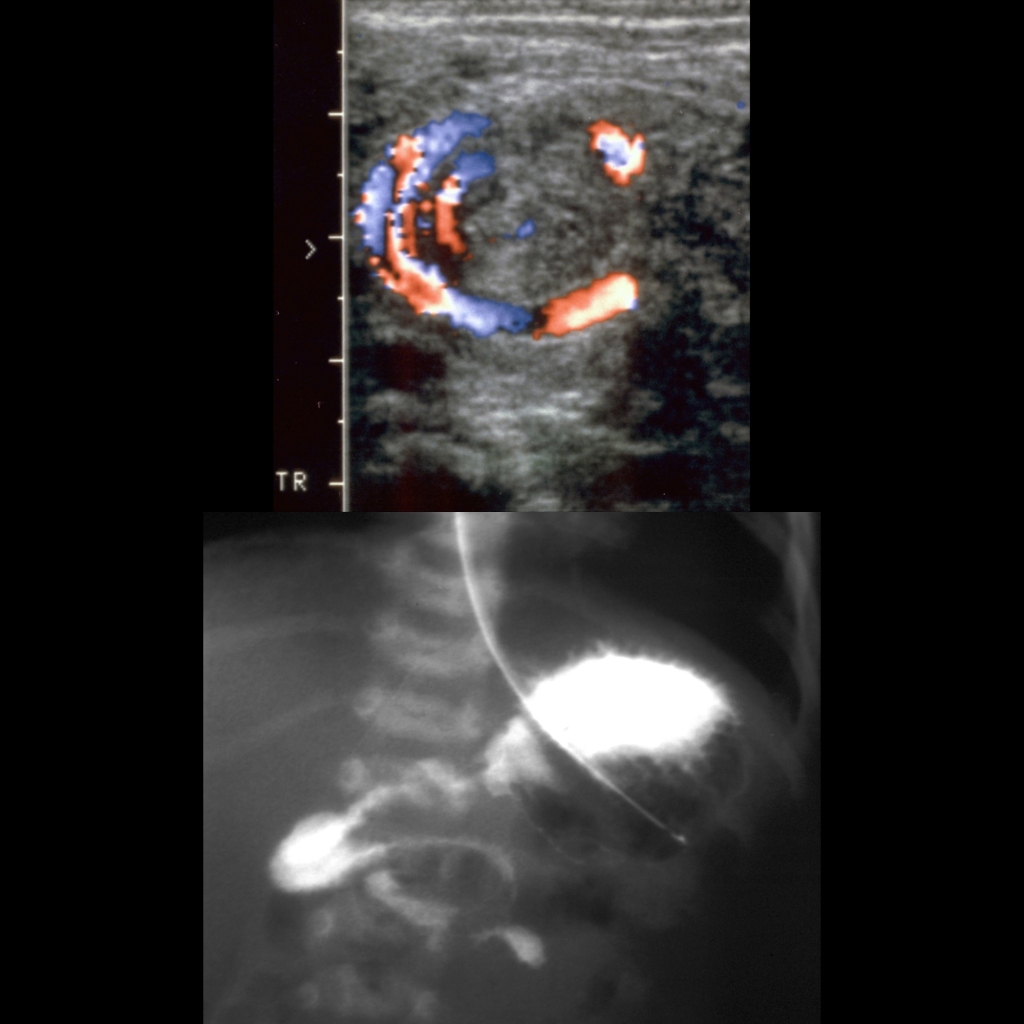
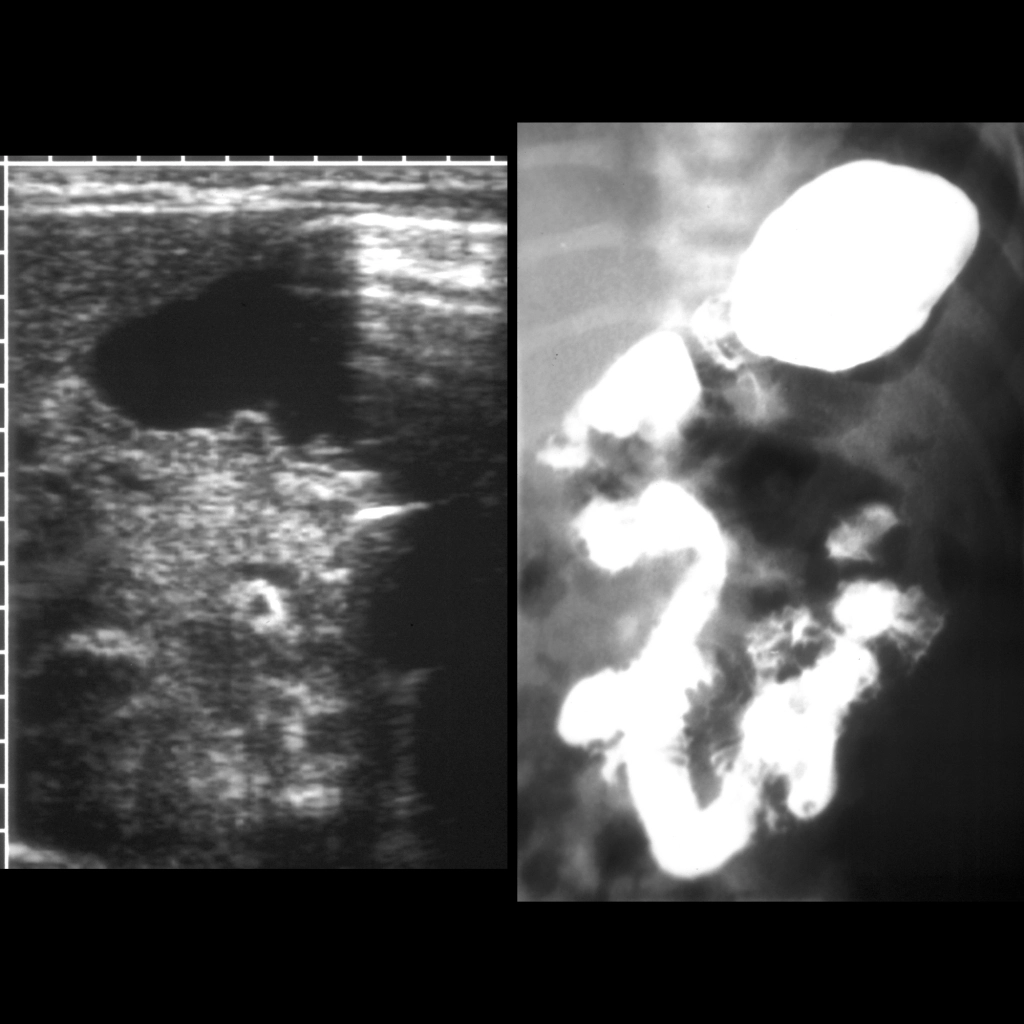
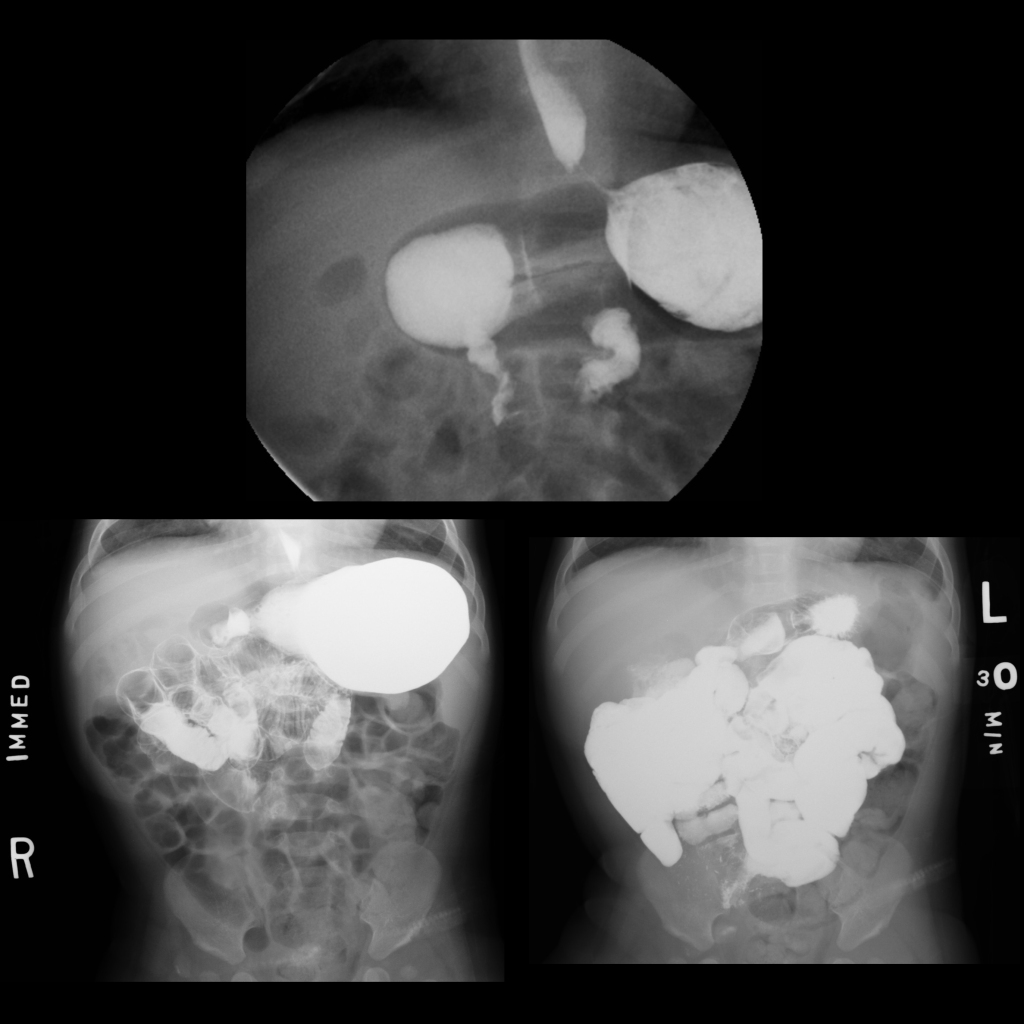
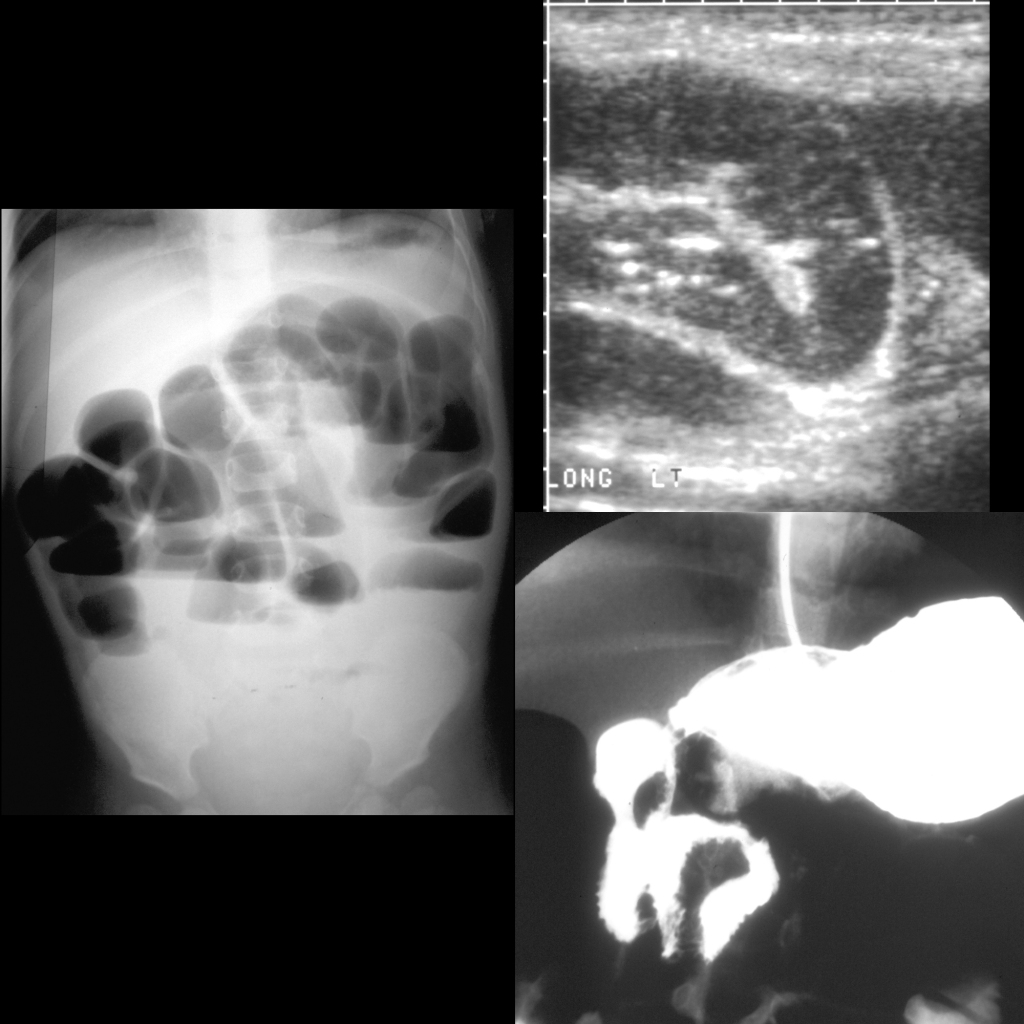
- US: reversal of normal relationship of superior mesenteric vein and superior mesenteric artery on axial images – super mesenteric vein is to the right of the superior mesenteric artery in the body, if the superior mesenteric vein is above or to the left of the superior mesenteric artery in the body should raise suspicion for malrotation being present, whirlpool sign – swirling of mesenteric vasculature around itself – is sign of midgut volvulus
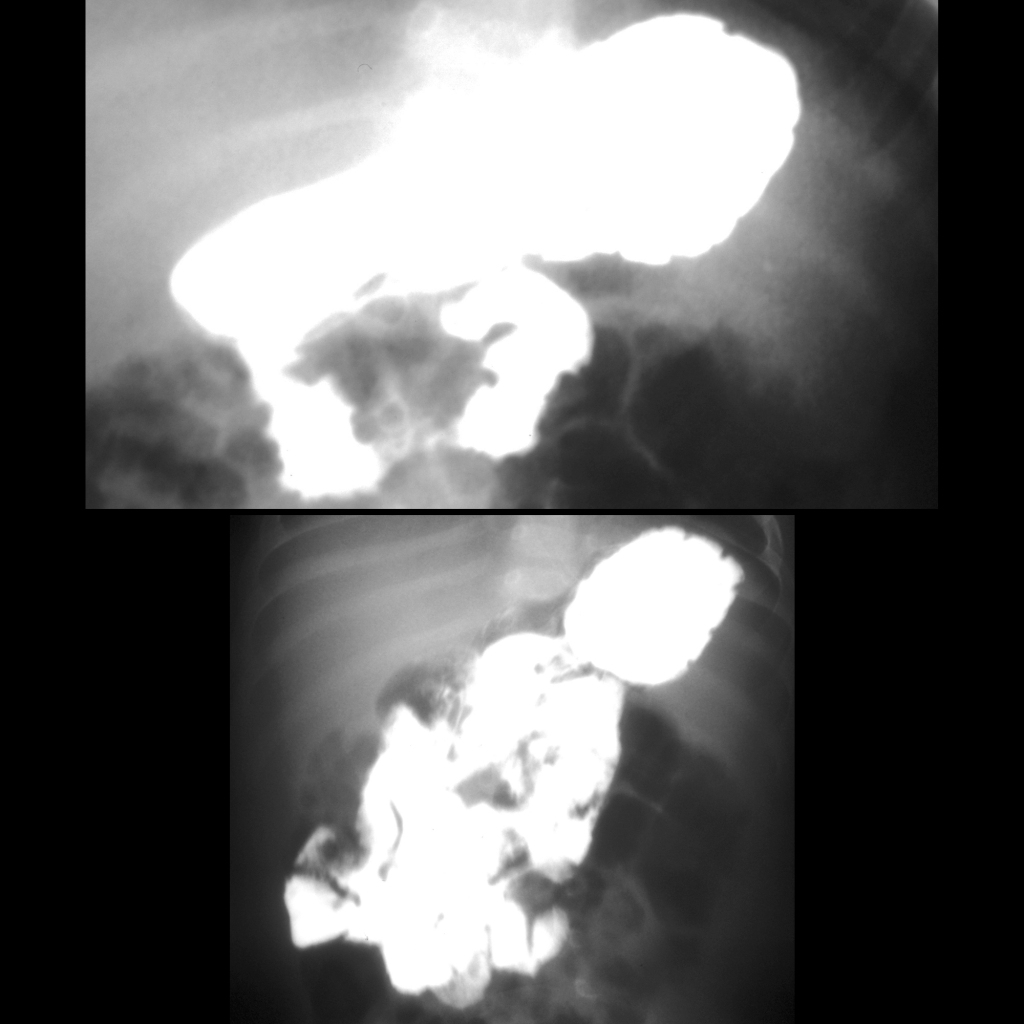
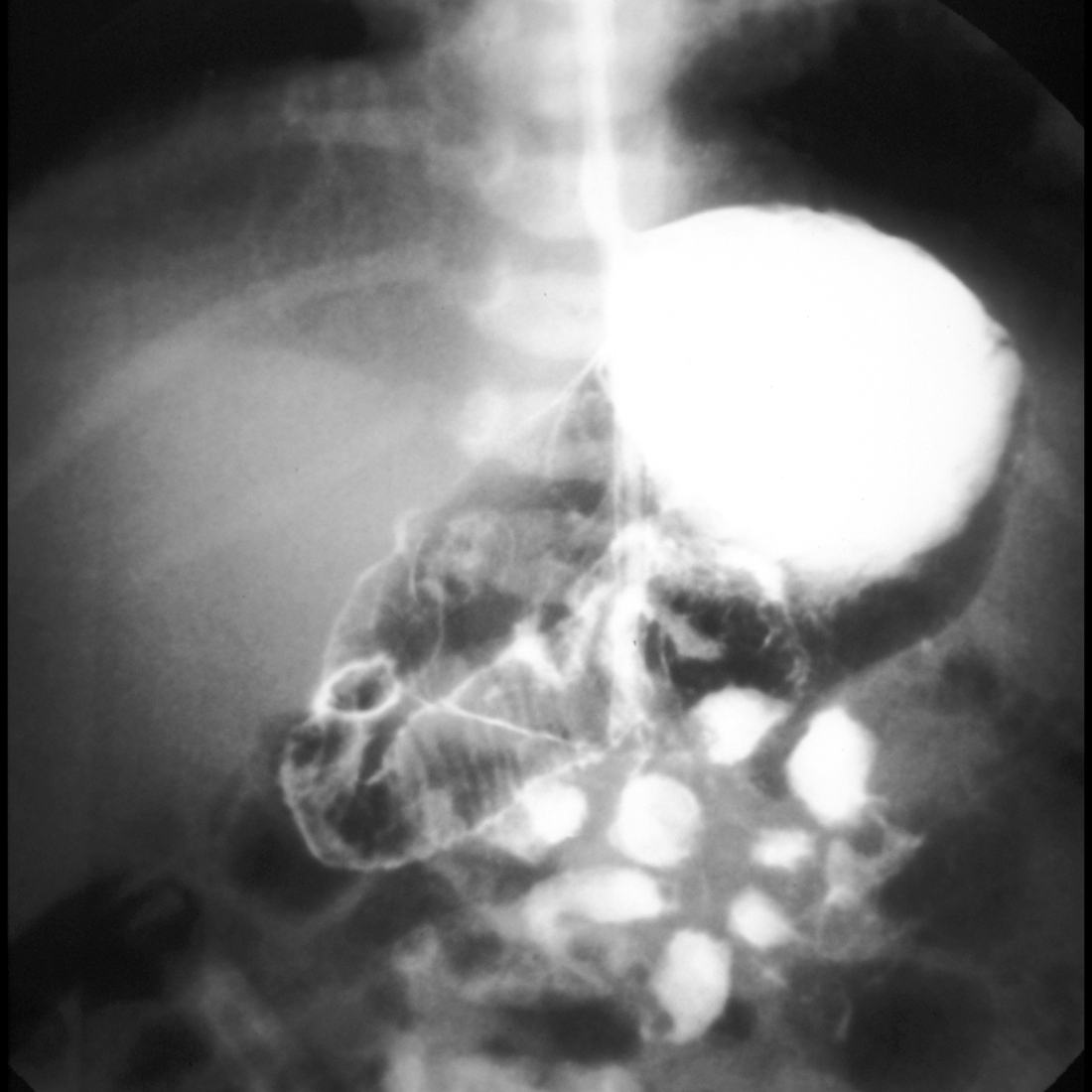
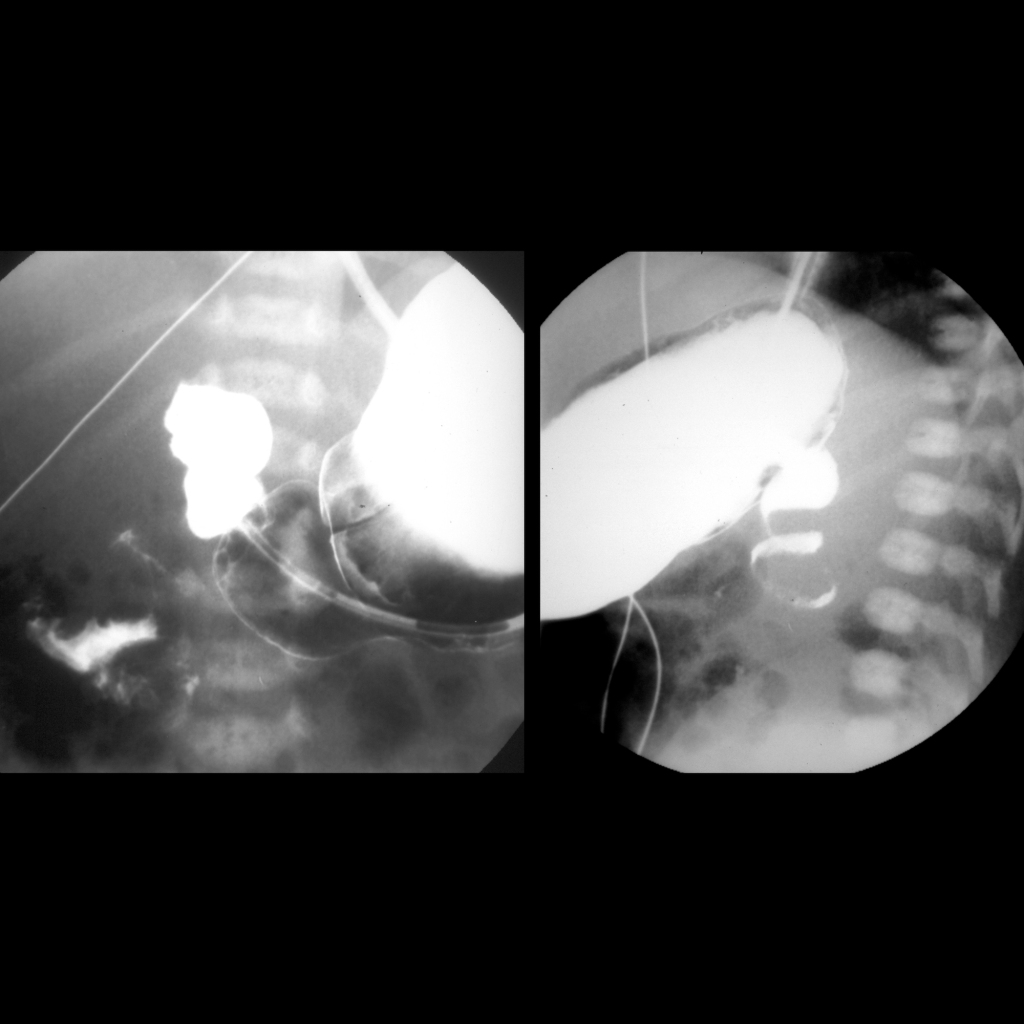
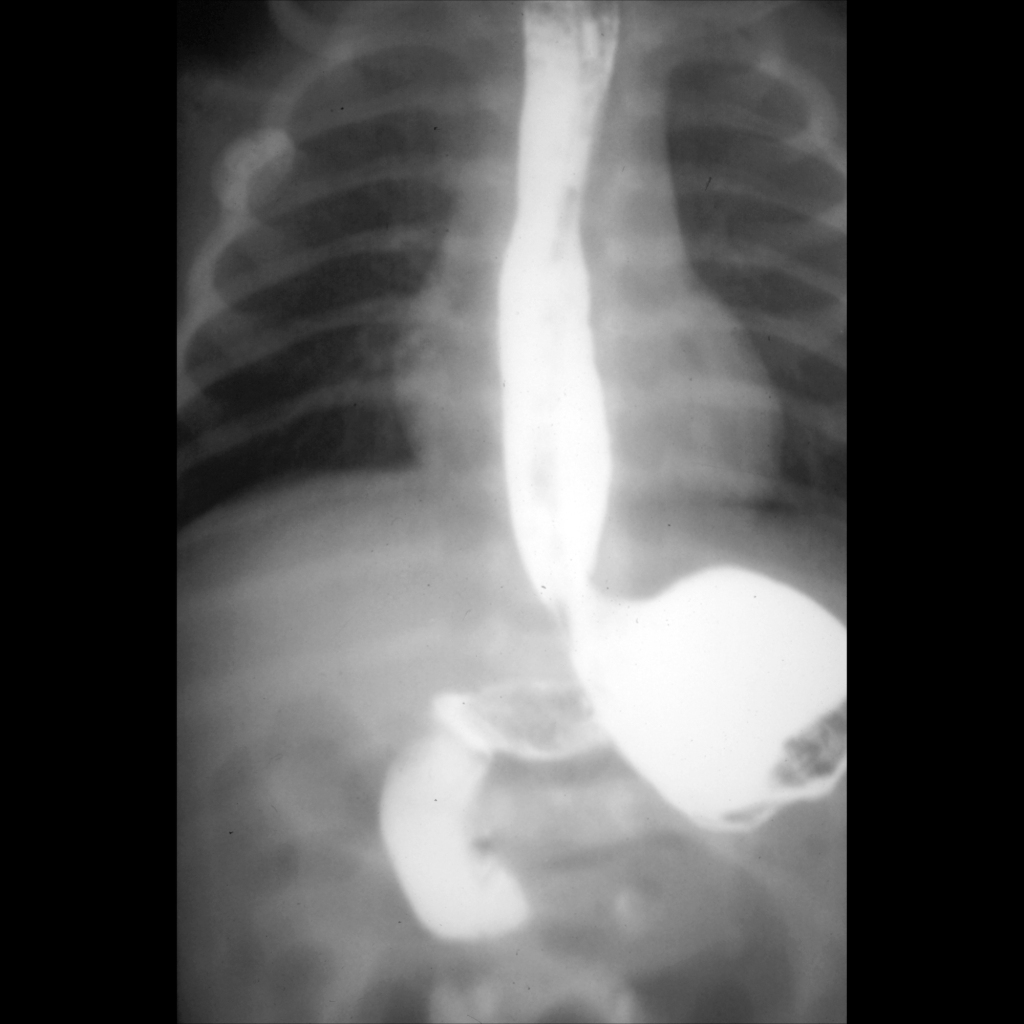
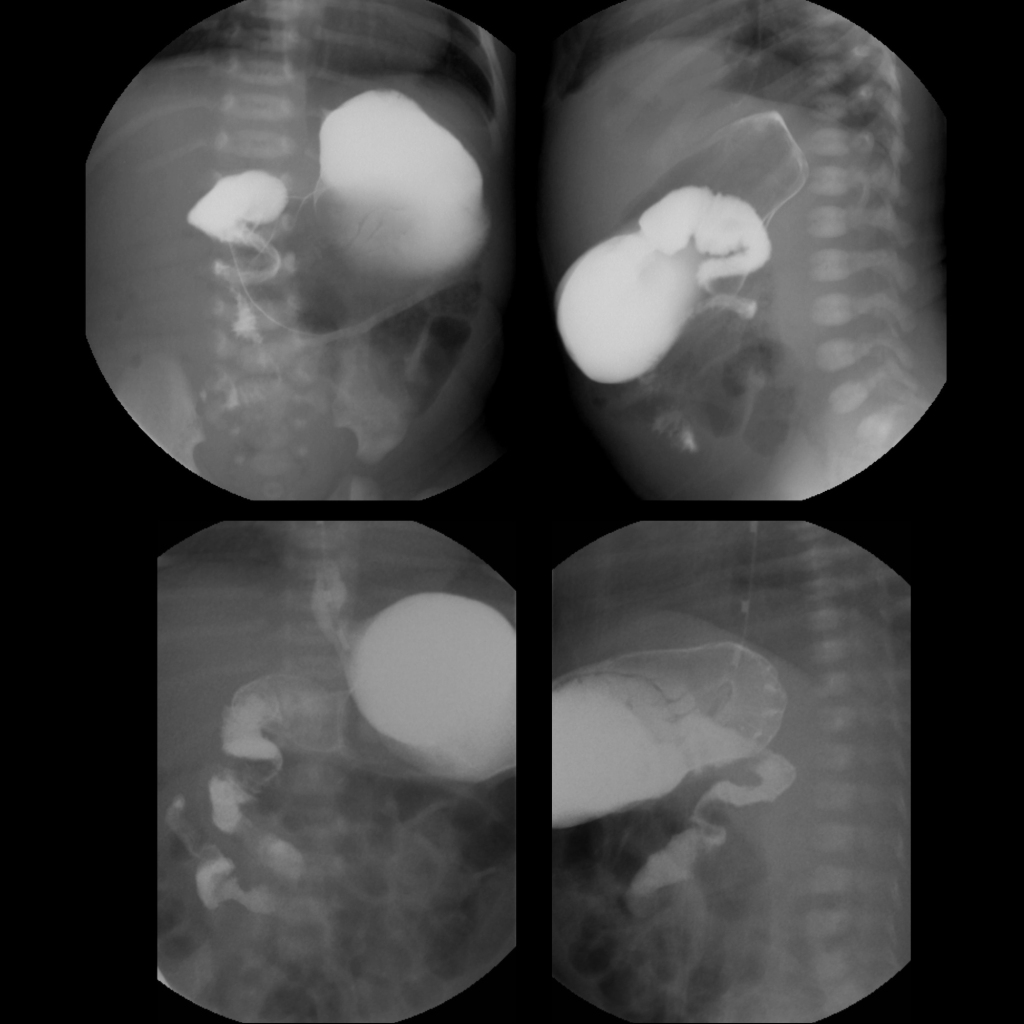
- UGI: duodenal-jejunal junction (ligament of Treitz) is where retroperitoneal duodenum comes out into peritoneum and it needs to be over left pedicle of spine or to left of spine and to be at level of duodenal bulb and failure to meet both of these criteria results in diagnosis of malrotation with small intestine in right side of abdomen and colon in left side of abdomen, often a spiral / apple peel / corkscrew appearance to the duodenum / proximal jejunum which is a demonstration of the volvulized bowel
- BE: abnormal position of cecum out of right lower quadrant either high in position in the right abdomen or anywhere on the left side of the abdomen should raise suspicion for malrotation being present, swirling of the terminal ileum is a sign of midgut volvulus
- Treatment: Ladd’s procedure
- Clinical: most occur early in life with 40% in first 10 days and 90% in first 3 months of life, bilious vomiting is radiological and surgical emergency as strangulation sequence can happen in few hours and time = bowel, in older children and adults may present as episodes of spontaneously resolving duodenal obstruction
Radiology Cases of Malrotation With Midgut Volvulus
Radiology Cases of Normal Bowel Rotation

Radiology Cases of Bilious Residuals After Feeding Due to Nasogastric Tube Malposition Clinically Mimicking Malrotation With Midgut Volvulus
Radiology Cases of Malrotation With Midgut Volvulus







Radiology Cases of Malrotation With Intermittent Midgut Volvulus

Radiology Cases of Malrotation With Midgut Volvulus Before and After Ladd Procedure
Radiology Cases of Malrotation With Chronic Midgut Volvulus

Radiology False Positive Cases of Malrotation With Midgut Volvulus
Radiology Cases of False Positive Cases of Malrotation With Midgut Volvulus Due to Displacement of the Duodenal-Jejunal Junction by Dilated Loops of Small Bowel
Surgery Cases of Malrotation With Midgut Volvulus











